The BDA and Wiltshire Farm Foods have partnered up to deliver a video that centres around the challenges of at home texture modification of meals. Many dietitians support service users who are recommended to try a texture modified diet for a period of time, but have you ever tried preparing a meal in this way or considered the impact of this on the wider family?
This video raises awareness of the practical implications of dysphagia for patients and their families, and includes important consideration of working in a Multi-Disciplinary Team (MDT). You’ll hear discussion from Dietitians, our members Alison Smith (read her experience and takeaways below) and Dysphagia Practitioner Laura Clarke, along with Speech and Language Therapist Dr Lindsey Collins, presented by Declan Henderson RD, to ensure our members and other healthcare professionals have takeaways they can then put into practice.
They are then challenged to put themselves into the patients' shoes by attempting to create their own IDDSI Level 4 Puréed meal.
The Ready, Steady, Blend Challenge
Watch Ready, Steady, Blend!
Alison Smith shares her Ready Steady Blend experience

The practicalities of puréeing food
As a dietitian who loves cooking and has had a long interest and involvement in nutrition and dysphagia, I thought I was ideally placed to take part in the Ready, Steady, Blend filming with Wiltshire Farm Foods. I am knowledgeable on the IDDSI descriptors, and I also know the theory about how to purée food but to my shame I’ve never actually tried preparing puréed food before, so I was really keen to take part in this challenge.
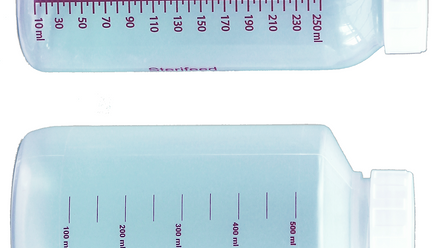
As it turns out, despite all my knowledge and understanding I found it really challenging to convert a single portion of a standard texture meal into a puréed meal that met all the IDDSI requirements for Level 4 which remained both palatable and nutritious.

So, my takeaways from this valuable experience are:
- Give it a try – it’s harder than you might think!
- Be honest with patients and carers about the challenges of producing the right texture puréed food
- Think about the equipment that patients and carers have access to
- A standard domestic blender or food processer isn’t much use unless you are puréeing large quantities of food
- A stick blender might be easier to use but again it works better with larger amounts of food
- Sieving food instead of blending is hard work
- Knowing how much liquid to add to a food to achieve the right texture is a case of trial and error, but the key is to add fluid sparingly so you don’t accidentally make the puree too thin
- If a single meal is being puréed, consider how each component can be kept hot while it is being prepared – a lukewarm meal is unlikely to be a palatable meal
- Puréeing a full meal takes time – much as I would never advocate it for so many reasons, I can see why carers might decide to purée all aspects of a meal together for speed

Other things to think about
It is always worth considering that just because a patient has been advised to have a puréed diet doesn’t mean that they have to follow that advice, or that we, as health care practitioners, have to make them follow it.
All adults with capacity have the right to make their own decisions, even if we consider their decision to be unwise. For adults who lack capacity to make a decision about whether to follow guidance about having modified texture food or fluid, the person’s best interests should guide decision making – and we need to remember that best interests don’t just mean what is considered safe; it also means what is acceptable to the patient. A good shorthand for this is a statement made by Justice Munby in 2007: “What is the point of making someone safe if by doing so we just make them miserable”.
When it comes to how to support care home staff, the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 helpfully states that “The nutritional and hydration needs of service users must be met [but this] does not apply [where] the meeting of such nutritional or hydration needs would:
- result in a breach of regulation 11 (Care and treatment of service users must only be provided with the consent of the relevant person)
- not be in the service user’s best interests”
Overall, I have really enjoyed reflecting on the skills and confidence needed to produce a puréed meal and I’d encourage you all to give it a go!
References
Health and Social Care Act 2008 (Regulated Activities) Regulations 2014. https://www.legislation.gov.uk/ukdsi/2014/9780111117613/contents