The Glycaemic Index (GI) shows how quickly carbohydrate foods raise blood glucose (blood sugar) after eating. This is useful to know if you have diabetes, pre-diabetes, gestational diabetes or Polycystic Ovary Syndrome (PCOS) as it helps you to manage your blood glucose levels.
What is the Glycaemic Index?
After a meal, any of the starchy or sugary carbohydrates eaten are digested in the gut and absorbed into the bloodstream, raising blood glucose levels.
Carbohydrates are present in a wide variety of foods that are important to include as part of a balanced diet. These include starchy foods like potatoes, grains, legumes, bread, cereals, oats, rice, and pasta and foods that contain added sugars such as cakes, sweets and desserts or natural sugars found in fruits (fructose) or milk and dairy products (lactose).
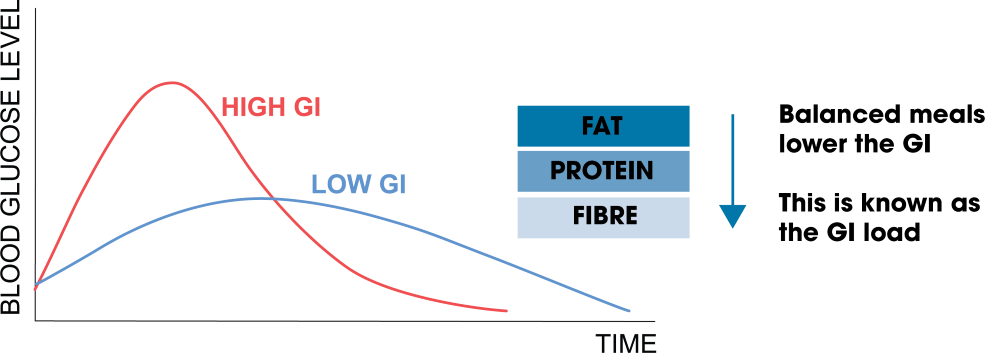
The Glycaemic Index (GI) shows how quickly foods increase your blood glucose level when you eat carbohydrates. Each food and drink have a score between 0 and 100. High GI foods (70 or above) cause a rapid rise in blood glucose, while low GI foods (55 or below) lead to a slower rise after eating. Protein, fat and fibre slow down digestion, so when eaten in combination with carbohydrate, the carbohydrate is absorbed more slowly and helps to prevent spikes in blood glucose levels.
High GI foods can be useful to consume if you live with diabetes and have a low blood glucose level that needs treating to bring your blood glucose levels up quickly.
So, what foods are considered low, medium and high?
| Carbohydrate | Lower GI | Medium GI | High GI |
| Bread | multigrain, granary, rye, seeded, wholegrain, oat, pitta, chapatti | crumpets, wholemeal | white bread, bagels, baguette, ciabatta |
| Rice | basmati, long grain, brown rice | risotto, wild rice | instant white rice, glutinous rice |
| Potatoes | new potatoes (with skins), sweet potato, yam | boiled potato, french fries | jacket potato |
| Pasta | all pasta cooked until al dente, noodles | macaroni, egg noodles | soft and over-cooked pasta |
| Other Grains | bulgar wheat, barley, quinoa | couscous, millet | tapioca |
| Breakfast Cereal | jumbo porridge oats, unsweetened muesli, most oat/bran-based cereals | wholewheat flakes mixed with a blend of dried fruits, toasted rice, wheat and barley flakes, puffed wheat, bran flakes, shredded wheat | instant oats, cornflakes, puffed wheat, wheat biscuits, wholegrain wheat malts |
How can a dietitian help you with managing GI?
If you are living with diabetes, have non-diabetic hyperglycaemia (pre-diabetes), gestational diabetes, or Polycystic Ovary Syndrome (PCOS), understanding GI can be beneficial in helping you manage your blood glucose levels. A dietitian can help you understand the impact of different foods on your blood glucose levels and support you to balance your meals and enjoy foods suited to your individual diet and lifestyle.
If you are taking any medications to manage your diabetes, please speak to your healthcare professional before making any changes to your diet.
Including lower GI foods in your diet in appropriate portion sizes can provide other health benefits. Choose less processed foods that are richer in nutrients and fibre. These are more filling and important for gut health and maintaining a healthy weight.
A high fibre diet might not be suitable for everyone however, such as those living with irritable bowel syndrome (IBS). Seek further support from a dietitian if you live with a condition that might make eating higher GI foods problematic.
If you are interested in following a low carbohydrate diet, speaking with a dietitian is important to ensure your diet doesn’t lack essential nutrients.
How can you eat with this in mind?
While the GI of carbohydrate foods is certainly a factor in how quickly blood glucose levels rise after a meal, it is not the only consideration.
The portion size of carbohydrate-rich foods often has the greatest impact. To limit the increase in blood glucose, choose sensible portion sizes and combine carbohydrates with other foods to slow down digestion.
For example, a jacket potato eaten on its own is considered a high GI food, but the impact on blood glucose can be reduced by keeping the skin on, adding a side serving of salad for fibre, tuna for protein and a small amount of mayonnaise for fat. This is known as the GI load.
Overall, it is important to focus on eating a nutrient-dense diet and consider foods such as wholegrains, legumes, vegetables and fruits. Include high-quality protein foods such as eggs, fish, poultry, lean meats, nuts and plant-based proteins like tofu. Use healthier fats in moderation, such as olive or rapeseed oils and avocado.
Top tips
- The total amount of carbohydrates in a meal has the most effect on your blood glucose levels. Keep portion sizes sensible. For most adults this is a fist-sized serving of a starchy food or making up a quarter to a third of your plate depending on how active you are.
- Choose wholegrain, higher fibre and no added sugar varieties of carbohydrates, as fibre helps to stabilise blood glucose levels, lowering the GI of the food.
- Aim to balance your meals by including good quality sources of protein such as lean meat, eggs or fish, or plant-based alternatives (beans, lentils, soya) and plenty of vegetables or salad.
- Take a gradual approach to increasing fibre in your diet. Fibre introduced too quickly can cause unpleasant gastrointestinal side effects. Look at the BDA’s Fibre Food Fact Sheet for further information and make sure you stay well hydrated.
- Aim to include more pulses such as lentils, chickpeas, beans and wholegrains like oats, brown or wild rice, barley, millet, corn, buckwheat, quinoa, spelt, freekeh and rye.
- Where possible, keep the skins on any fruit, vegetables or potatoes to increase the fibre content.
- Riper and more tropical fruits such as yellow or brown bananas, mango and pineapple will raise blood glucose levels more quickly. Aim to choose less ripe options, include more locally grown fruits such as berries and if eating tropical fruits, limit your intake to around an 80g serving and spread your fruit intake out.
- Cooking methods can also influence the GI of foods. Softer pasta has a higher GI than al dente pasta. Cooked and cooled starchy foods such as potatoes, pasta, beans and rice used in salads also have a lower GI. Freezing and toasting bread has the same effect.
- Limit your intake of added sugars from cakes, biscuits, sweets, chocolate, crisps, puddings and desserts as these contain high amounts of fat, sugar, and salt. Make healthier snack swaps such as fruit and nuts in sensible portions or chopped vegetables with houmous.
- Swap sugary drinks for water or herbal tea. Be mindful of hidden sugars in fresh fruit juice and smoothies. Limit fruit juice to no more than 150ml per day and choose vegetable-based smoothies.
Source(s)
Warren JM, Henry CJ, Simonite V. Low Glycaemic Index Breakfasts and Reduced Food Intake in Preadolescent Children. Pediatrics. 2003 Nov;112(5):e414.
Govindji A, Puddefoot N. The GI Plan Random House Publishing, 2004.
https://ec.europa.eu/food/safety/labelling_nutrition/claims/register/public/?event=register.home
https://www.asa.org.uk/advice-online/weight-control-glycaemic-index-gi.html
https://www.nature.com/articles/1601454
The graph in this food fact sheet was reproduced with kind permission of www.glycaemicindex.com







