Rebecca Fisher and Alison Smith introduce improved categorisation in the ePACT2 primary care prescribing data platform.
Data – it’s a big deal these days. We are bombarded with an array of data in our everyday lives and collecting data is big business. But what data do we have access to in and about dietetics? As we go ever-increasingly digital, dietetics should not be left behind.
Up until now, our options have been rather limited to what is collected routinely by government or what we collect and collate ourselves e.g. British Artificial Nutrition Survey. Availability and access to pertinent data has never been more important but it can be hard for our profession to access meaningful national data. Until now!
The NHS Business Services Authority publishes primary care prescribing data via a platform called ePACT2. This source of data can be used to create dashboards and metrics to tell a story or to support monitoring of clinically- and cost-effective prescribing. The platform isn’t new, and if you have previously looked at prescribing information on openprescribing.net, you may be thinking “So what?” What are new, are the improved categories and categorisation of products within ePACT2.
As part of a move towards interoperability and data-driven care, the Department of Health and Social Care and NHS Business Services (NHS BSA) have worked together, supported by NHS London Procurement Partnership and specialist dietitians, to recategorise all nutritional borderline substance products.
Until now, the ability to analyse nutrition prescribing data has been extremely limited unless time-consuming, bespoke searches were created by medicines optimisation pharmacists or dietitians. For example, it was not a simple process to compare something as obvious and theoretically simple as the ratio of prescribed amino acid infant formula with extensively hydrolysed infant formula.
The NHS BSA is also supporting development of dashboards on key areas of interest relating to prescribed nutritional borderline substances.
Dispensing data from ePACT2 does not just include the items issued to the patient, but can be considered as part of a richer picture of population health through use of demographics including age, sex, and additional need factors such as deprivation, social housing and mortality ratio. This can help us to understand differences in prescribing within and between areas, enabling identification of areas where high use is to be expected or where further investigation may be needed (so-called warranted and unwarranted variation).
Something that crops up in audits within GP practices is the frequency of older adults inadvertently being prescribed infant formulas. This is such a wasted opportunity to manage undernutrition effectively.
Colleagues at NHS England Commercial Medicines Unit have reviewed recent prescribing trends for our highest cost areas of prescribing (see Figure 1) which gives pause for thought on the financial sustainability of nutrition prescribing.
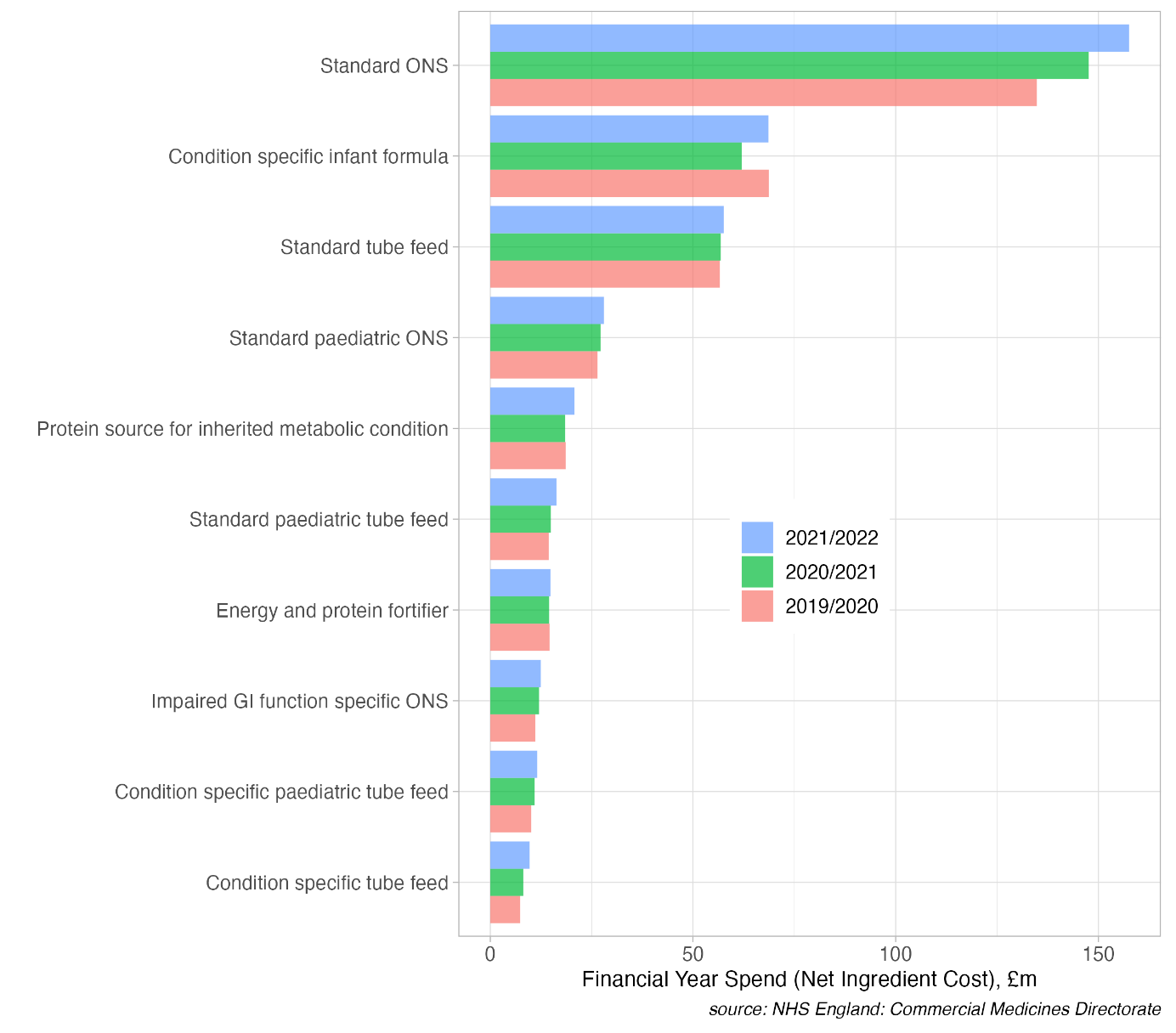
Figure 1. Prescribing trends for ACBS products
Dietitians interested in exploring data for their patients can look into the Digital Competency Framework for AHPs (domain 2 data management and clinical informatics) and the training available, listed in annex D of the pharmacy equivalent document. Dietetic teams can contact their local prescribing support dietitian to better understand local prescribing data and the Optimising Nutrition Prescribing Group is keen to support other specialist groups in understanding data for their clinical area.
With special thanks to the Commercial Medicines Unit and all the specialist dietitians who have supported this work.







