Elaine Anderson RD, Freelance and NHS Dietitian, discusses the low histamine diet, whether it can help alleviate Long Covid symptoms and why you should get support from a dietitian.
Long Covid
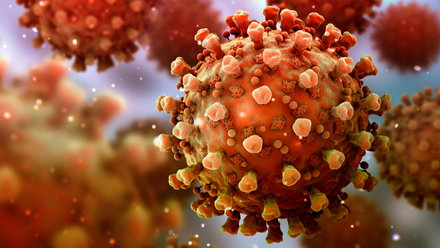
Long-COVID is defined as “symptoms that develop during or following an infection consistent with COVID-19, continue for more than 12 weeks and are not explained by an alternative diagnosis”1.
For several months, scientists have been considering the role of mast cell activation syndrome (MCAS) in COVID-192.They suggest that in some individuals, COVID-19 could lead to the development of MCAS, where the mast cells release histamine in response to the viral infection3 and that this dysfunctional response of mast cells may be an important consideration in cases of severe COVID-19 infection and chronic post-COVID-19 illnesses.
What is histamine?
Histamine is an inflammatory substance produced by cells in the body during an infection. It encourages an immune response to help fight off viruses and bacteria. Histamine also occurs naturally in foods.
Histamine Intolerance
Most people tolerate the amount of histamine found in an average diet4. Some people may be affected by histamine present in food. This is thought to be due to a reduced activity of the enzyme called diamine oxidase, which breaks down histamine5,6. This can then lead to an increased amount of histamine in the body and histamine intolerance. However, evidence for this has yet to be demonstrated7.
Histamine intolerance symptoms include headache, asthma, runny or blocked nose, low blood pressure, irregular heartbeat, hives, itching, diarrhoea, flushing and other conditions4
Symptoms can occur after a few hours up to a few days after eating foods high in histamine8. These symptoms are similar to those reported by people living with Long Covid.
Diagnosis of Histamine Intolerance
As yet, there is no test that can diagnose histamine intolerance. It is not a food allergy; therefore, food allergy testing is not helpful. The best way to investigate histamine intolerance is to avoid high histamine foods for approximately 2-4 weeks. Then, reintroduce gradually to assess tolerance6. This should be under the supervision of a registered dietitian.
It may also be advisable to have a clinical assessment with a medical doctor. Ideally, one who is experienced in histamine intolerance (or Mast Cell Activation Syndrome). They can also consider other tests to exclude other conditions.
Current practice/research
A small number of medical doctors are suggesting a low histamine diet to help with Long Covid symptom, however currently, there is a lack of evidence to support this. The government has given £18.5 million to fund research projects to help better understand the causes, symptoms and treatment of Long Covid. At present, there is no research specifically addressing the low histamine diet9.
There have been some case reports of successful treatment of MCAS with a low histamine diet along with other treatments10. There have also been several anecdotal reports through the long covid community. It is important to stress that there is not enough evidence to suggest this will be helpful for everyone.
The low histamine diet
Following a low histamine diet involves avoiding food and drink such as11:
- Tinned, fermented or pickled fish
- Fermented dairy such as aged cheese
- Cured or processed meats
- Fruit and vegetables such as oranges, bananas, spinach and tomatoes.
- Wine and beer
- Some nuts such as peanuts and tree nuts
Eating fresh foods over ready meals or food that has been stored for longer periods is also advised. This is due to the potential of higher histamine levels. A significant amount of organisation goes into ensuring a low histamine diet. This can troublesome if fatigue and memory problems are also an issue.
Some research suggests that some foods stimulate the release of histamine in the body. There is still no evidence that these foods have a clinical significance12.
Difficulties with a low histamine diet
A low histamine diet can be restrictive and time-consuming. Feedback from the Long Covid support groups suggest that many have tried the diet but found it difficult to follow combined with their debilitating symptoms.
There are also many food lists available on the internet and many have conflicting advice.
In addition, histamine levels in food can have a significant variation. Histamine levels are subject to the age of the food, the storage time, and how it has been treated7. This can cause issues establishing actual histamine content in foods.
Medications
Some studies report that some medications and alcohol can inhibit the enzyme diamine oxidase (DAO). This enzyme helps break histamine down in the body, however further research is also needed in this area12.
Why work with a dietitian
A dietitian can assess your food diary and advise if you may benefit from a trial of a low histamine diet. It is important to work with a dietitian as the low histamine diet can be limiting and may lead to nutrient deficiencies if followed for long periods.
A dietitian will ensure adequate nutrition during the restriction phase and support when re-introducing foods. Some individuals may be able to tolerate a certain amount of histamine in their diet after a period of time.
Some individuals may need further medical support such as medications like antihistamines or mast cell stabilisers which would be prescribed by a specialist in the area.
If the low histamine diet is not suitable or indicated then a dietitian can also look at other components of the diet and give tailored, practical advice to help with symptoms.
Conclusion
Dietitians can support concerns around histamine intolerance and long covid. They are the only health professionals to be regulated by law, and are governed by an ethical code to ensure they always work to the highest standard13.
Recently, the Food Allergy Specialist Group of the BDA has produced guidance for dietitians on this subject due to the lack of evidence available. Despite the absence of research, dietitians are encouraged to be supportive and respectful of a person’s decision to trial a low histamine diet if that is what they choose to do.
It is important that this diet is only followed for a short period of time. This is vital to help decrease the possibility of long-term restrictive diets, which can lead to poor health outcomes and a reduced quality of life7.
If you are looking for more information you can visit the NHS Your Covid Recovery website or our own advice on Diet and COVID-19. You can also read the BDA Food Allergy Specialist Group's short guidance document on low histamine diet.
References:
- NICE, SIGN & RCGP. COVID-19 rapid guideline: managing the long-term effects of COVID-19. December 2020. Available from: Overview | COVID-19 rapid guideline: managing the long-term effects of COVID-19 | Guidance | NICE
- Afrin LB, Weinstock LB, Molderings GJ. Covid-19 hyperinflammation and post-Covid-19 illness may be rooted in mast cell activation syndrome. Int J Infect Dis. 2020 Nov;100:327-332.
- Kritas SK, Ronconi G, Caraffa A, Gallenga CE, Ross R, Conti P. Mast cells contribute to coronavirus-induced inflammation: new anti-inflammatory strategy. J Biol Regul Homeost Agents. 2020 January-February,;34(1):9-14.
- Laura Maintz & Natalija Novak, Histamine and histamine intolerance, The American Journal of Clinical Nutrition 2007, May, Volume 85, Issue 5 Pages 1185–1196
- Comas-Basté O, Sánchez-Pérez S, Veciana-Nogués MT, Latorre-Moratalla M, Vidal-Carou MDC. Histamine Intolerance: The Current State of the Art. Biomolecules. 2020;10(8)
- Allergy UK Your Quick Guide to Histamine Intolerance Accessed May 2021 Available from: Histamine_Intolerance_original_original (5).pdf
- Reese, I., Ballmer-Weber, B., Beyer, K. et al. German guideline for the management of adverse reactions to ingested histamine. Allergo J Int 2017, 26, 72–79 Available at: https://doi.org/10.1007/s40629-017-0011-5
- Pinzer, T C et al. “Circadian profiling reveals higher histamine plasma levels and lower diamine oxidase serum activities in 24% of patients with suspected histamine intolerance compared to food allergy and controls.” Allergy vol. 2018, 73,4: 949-957.
- Gov.UK Press Release £18.5 million to tackle long Covid through research 2021, Feb Available from: £18.5 million to tackle long COVID through research - GOV.UK (www.gov.uk)
- Schofield JR. Persistent antiphospholipid antibodies, mast cell activation syndrome, postural orthostatic tachycardia syndrome and post COVID syndrome: 1 year on. EJCRIM 2021;8 Available at doi:10.12890/2021_002378
- Skypala IJ, Williams M, Reeves L, Meyer R, Venter C. Sensitivity to food additives, vaso-active amines and salicylates: a review of the evidence. Clin Transl Allergy. 2015 Oct 13;5:34
- Vlieg-Boerstra BJ, van der Heide S, Oude Elberink JN, Kluin-Nelemans JC, Dubois AE. Mastocytosis and adverse reactions to biogenic amines and histamine-releasing foods: what is the evidence? Neth J Med. 2005 Jul-Aug;63(7):244-9.
- BDA Dietitian or Nutritionist? Accessed May 2021: Dietitian or nutritionist? (bda.uk.com)