Nasogastric tube feeding can be an important tool for treating malnutrition. Phill Johnston wanted to find out more about the patient experience so had an NG tube fitted as part of Nutrition and Hydration Week 2020.
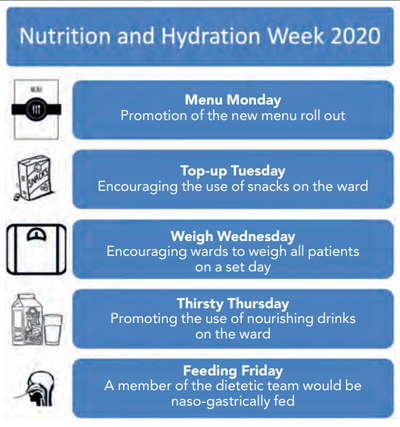
Nutrition and Hydration Week is a yearly event designed to promote the importance and optimisation of nutrition and hydration. At Royal Stoke University Hospital, this is an event routinely taken up by the dietetic department to engage all members of staff in ensuring the patients we meet on a day-to-day basis have the optimal nutritional status. As a result of this the department had set five different themes for each day of the week (Figure 1).
The majority of these ideas were to be promoted using stands in two of the main walking routes in the hospital. For me working on a stand is an idea that takes me out of my comfort zone – I am an individual who would avoid eye contact with stand workers to avoid been drawn in. The experience of being naso-gastrically-fed, I thought would be invaluable.
One of my colleagues originally opted to be fed, however two nasogastric (NG) insertions failed due to being unable to obtain an aspirate. A third was successfully inserted and aspirated by one of the ear nose and throat consultants, however after constant gagging and vomiting with feed, the NG was removed. This provided an invaluable learning point, as I have seen many patients who have had NGs inserted and patients have informed me they simply could not tolerate it and removed it. My usual response has been to persevere and assume that it cannot be that bad, however my colleague looked genuinely unwell.
4 years since my 4 days of #NGfeeding
— Phill Johnston (@PhillJohnstonRD) March 18, 2024
One of the best and most most enlightening experiences of my #dietetic careerhttps://t.co/GF2vrLjAGd
It also means 4 years since i met my first COVID patient. Who knew what was to come@BDA_Dietitians @SCODietitians @NCAlliance_NHS pic.twitter.com/9XZel0kB1g
After the promotion made by the team, I felt it would be a disappointment for this not to go ahead and I volunteered for insertion on the Tuesday. My original intention was to be nil by mouth and fully fed and hydrated for one week post insertion. Unfortunately, Nutrition and Hydration Week coincided with the COVID-19 breakout, meaning plans soon changed.
Background
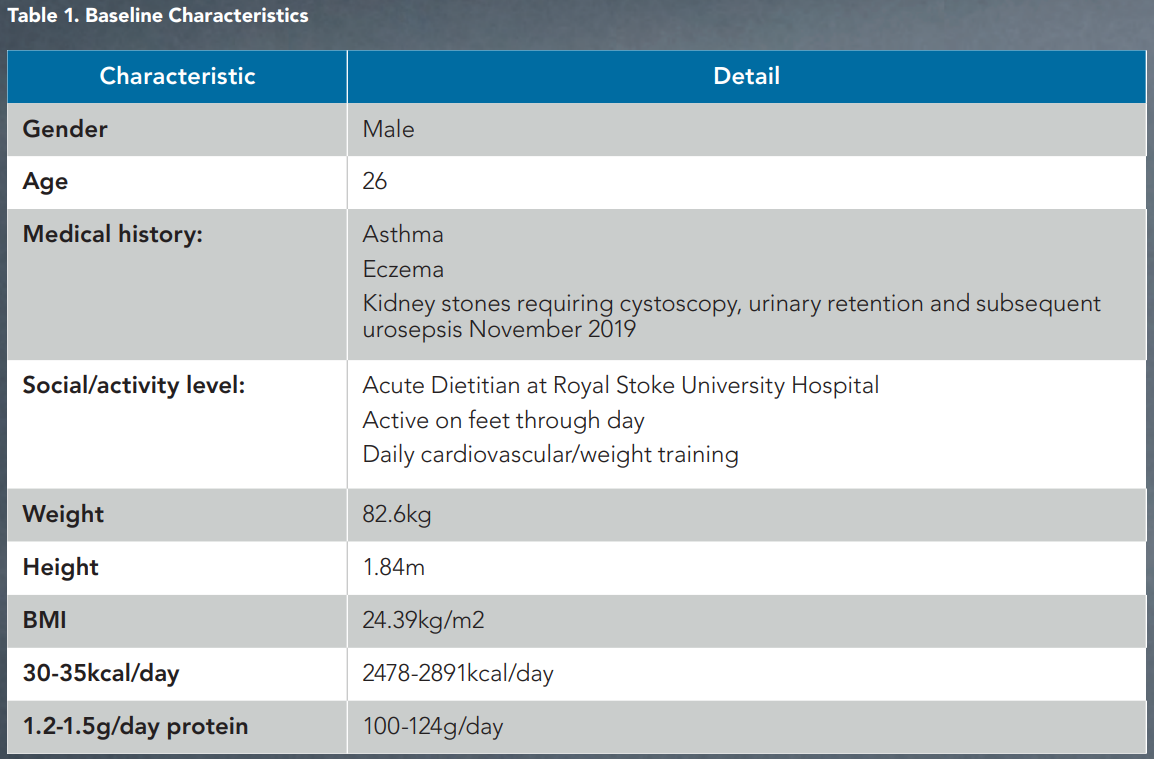
Baseline characteristics are provided in Table 1. I estimated my calorie and protein requirements via a simplistic amount per kilogram method with the intention of monitoring my weight daily and adjusting intake as needed.
Placement
As I am sure is the case with any dietitian, I have my go-to nursing staff for NG-related issues and fortunately one of the nursing team was available for NG placement on the Tuesday morning. I had an 8fr NG successfully inserted in a single attempt. Insertion was much less unpleasant than I imagined, however I was of the mindset that nothing could be worse than a catheter. The NG was inserted with a few sips of water with the main discomfort being a runny nose and the eye adjacent to the NG streaming. The first hours after insertion were uncomfortable.
My throat felt constantly irritated and every few minutes there was a feeling of the NG coiling in the back of my throat. I felt I would need to do a large swallow to alleviate this. If I spoke in long sentences or turned my head quickly I would start to gag. My nose felt it was permanently running and the need to blow my nose or sniff was constant. This was heighted by the COVID-19 outbreak and every need to touch my face felt it needed to be additionally justified. Speaking after insertion, I felt I was very nasal and listening back to my first day of the video diary confirms this.
In all honesty, for the first few hours with the NG, I was miserable. It provided me with a completely new understanding of why so many patients I see have had their NGs “fall out” in the first 24-hour period. Going to bed that evening I thought if the tube were to fall out overnight I would not be too disappointed. Surprisingly, I slept much better than I expected. Once I was awake, almost all the irritations of the day previous had passed and I was able to hold a conversation and move my head without discomfort. The only feeling that lasted was that of a runny nose, however I think this was more due to the plaster on my nose being damp than actually running.
I have said to many patients in the past that insertion and the first few hours with the NG are the most difficult, but if they get past the 24-48 hour mark then the tube softens and the discomfort passes. It was highly reassuring to know that this advice is accurate. Apart from seeing the plaster in my peripheral vision, I wouldn’t have known the NG was in place.
Throughout I wanted to keep in my normal work and social life, including attendance at ward rounds, reviewing patients and exercise. The NG became a talking point amongst colleagues and got other professionals thinking what they could do in their roles to provide a patient experience.
The overwhelming response to the NG was positive. Mostly these were comments on the commitment of putting myself through a procedure that so many professionals find unpleasant to think about or even discuss. Those not aware of my intentions showed genuine concern for my health, although there were a very small number of individuals who questioned if this was good clinical practice or why I didn’t research the evidence already in place. This response surprised me as I cannot understand why, as professionals, we would not want to get into the thought process of our patients and understand their barriers to feeding.
Outside of work I initially did feel self-conscious and it felt – over the first few days especially – I was getting a lot of double takes. However as I got more confident throughout the days, this appeared to diminish. I continued to exercise with a combination of running, elliptical and weight training and didn’t find any of these activities were impacted by the NG.
Feeding
Due to the resources I had available I opted for bolus feeding. I was using the Abbott range of ONS due to my workplace being contracted to Abbott and my familiarity with their product range. My thought process with feeding was that I wanted the minimal amount of feed for maximum benefit. I elected for eight Ensure Compacts per day (125ml, 300kcal, 12.75g protein/bottle) with 120ml water pre and post bolus (1920ml) with additional top up flushes as needed. Following my first feeding attempt, this changed due to the difficulty and time commitment of using such a viscous product. The first feed took nearly 30 minutes, so I decided to swap to seven Ensure Twocal (200ml, 400kcal, 16.8g protein/bottle). I was surprised by the difficulty and time commitment of bolus feeding and I would imagine any frail individual would struggle to manage bolus feeding with a fine bore tube.
I soon found the level of difficulty and amount of organisation needed to feed. After setting up my feed area and collecting my syringes, feed and water I found I had no pH strips, requiring a return to the wards to find some. My first use of the NG was for water. This had more effects than I imagined. I could feel the water from the tip of my nose all the way into my stomach, providing a sensation of if I were actually drinking.
Additionally, I found I was still highly salivating (although I imagine this was normal levels of salivation which would be masked when eating and drinking normally), which did provide a thirst-quenching effect in my mouth. I did find this initially difficult to manage as felt I had to make a conscious effort to time my swallow with having the original discomfort of the NG.
The high importance of organisation was again demonstrated when I went to the gym after work and forgot to take any syringes or pH strips, meaning my afternoon session was cut short to avoid any possible dehydration.
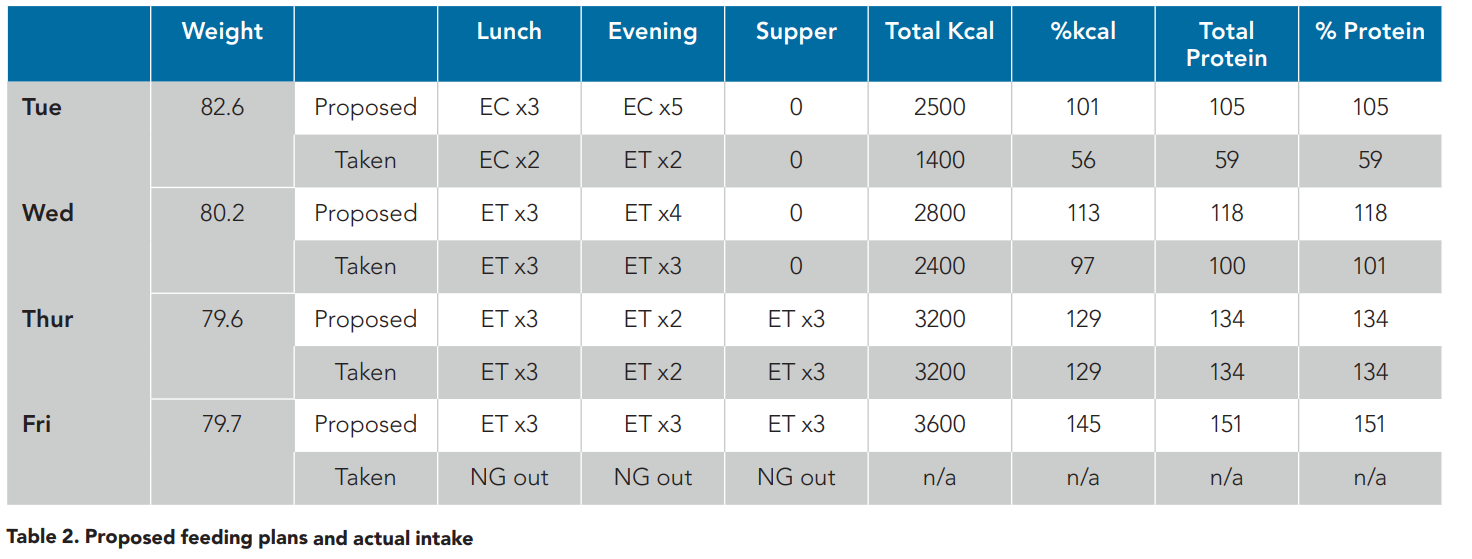
Table 2 displays my proposed feeding plans for the day compared to what I actually took in addition to my weight trends. Whilst I would like to say every day I achieved my intended feeding plan, this was not the case in the first few days. This was mostly due to the time commitment feeding was taking and the initial discomfort I experienced. I was very conscious, especially in the first day, of having too much feed mostly due to the gagging sensations I was still experiencing and my preference to avoid vomiting.
Whilst the time commitments may not sound great, I was taking no joy from feeding and I was originally struggling with discomfort. As an individual who greatly enjoys their food and normally has a very good appetite, the realisation of not eating was disheartening. Even on day one when my intake was low, I do not recall feeling hungry throughout my days of being NG-fed. I found it was more the sensation and flavours of eating I was missing rather than anything else.
My weight reduced on the first day of feed by 2.4kg. This appeared to be a drastic drop for one day of feeding, even with such a large nutritional deficit. From this, I intended to increase my overall calorie intake by 300kcal (34kcal/kg) and protein intake by 13g (1.4g/kg).
The second evening I hosted a live Facebook feed to demonstrate the time commitments of the practicalities of NG feeding. This was well received and promoted further interest in the practicalities of feeding. I was surprised by the amount of mess feeding could produce, even when being cautious. My hands would soon become sticky making plunging difficult. Additionally removing the foil lids from supplements became increasingly difficult. This further highlighted the needs of considering the effects of frailty when designing feed regimens for patients.
Despite increasing my total intakes, my weight reduced by a further 0.6kg. I further increased my nutritional targets for the day by 400kcal (39kcal/kg) and 29g protein (1.6g/kg). Due to time commitments of commuting and not liking to exercise on a full stomach, fitting in a breakfast feed was not an option for me. I instead decided to split my evening feeds into an evening meal and a supper.
On day three, I also had to re-evaluate my fluid intake as I found I was getting too dehydrated and my urine was too dark for my liking. Trying to maintain my caseload and fit in all my fluid needs was proving to be problematic and I could not justify taking myself away from ward rounds or working needs to test pHs and administer a water bolus. I therefore allowed oral fluids at work and for the gym, however, at home I remained NBM. This appeared successful and I gained 0.1kg, suggesting this regimen would be sufficient for weight maintenance.
I still wanted to gain weight and further increased targets by 400kcal (44kcal/kg) and 17g protein (1.8g/kg). On the Friday morning, as I was reviewing a patient I was informed they had tested positive for COVID-19. I took the decision to remove the NG as I could not justify keeping anything unnecessary in situ during a serious health pandemic. I felt an enormous sense of shame for ending my experiment this way, but I could no longer justify to myself that it was the right time to continue. The NG removal was surprisingly straightforward with nil discomfort.
Missed opportunities
It is hard not looking back with some disappointment as I had wanted to trial several other experiences whilst having the NG in. I would have liked to have trialled pump feed and pump-assisted bolus feeding. I think these methods of feeding would have suited my lifestyle much more than bolus as I feel the time commitments needed would be much less. I wanted to trial eating various modified texture diets to see how this may have impacted my appetite and my willingness to eat. I was also keen to trial alcohol down the NG to see the effects this may have had. Initially this was not on my to-do list, but I had numerous questions about trialling this and was keen to try and assess impact.
Bowels
As I am sure many dietitians are, I was interested to know the effect enteral feeding would have on my bowels. My bowels are normally twice daily routinely. The only real change to my bowel functions were that a couple of hours after lunch I would get an intense stomach pain and I would need to walk this off. I had no issues with feeding in the evening and I am unsure why I experienced afternoon symptoms.
Conclusion
I am very aware my time being home enterally-fed was very brief and there are individuals for whom this will be lifelong, however this has been hugely insightful. Mostly that the first 24 hours of feeding are difficult and patients may require increased input and discussion to help them get through this period. I kept a regular video diary which was posted on our UHNM Dietetics Twitter page, and a video was also posted on the UHNM Facebook page to raise awareness and conversation around enteral feeding. I also made a short video from my video diary to highlight how NG feeding works and the difficulties patients may encounter. You can watch this at the top of the page, or here.

