Evidence based practice (EBP) is at the core of nutrition and dietetic practice. It is important that all members of the nutrition and dietetic workforce understand what is meant by EBP, and that it is embedded into your practice.
The term evidence-based practice (EBP) evolved from the original term evidence-based medicine (EBM) which is a concept that was first introduced in the field of medicine during the early nineties.
In 2005, the term evidence-based practice (EBP) was introduced by a international working group who published ‘The Sicily statement on evidence-based practice’. This statement provided the following definition:
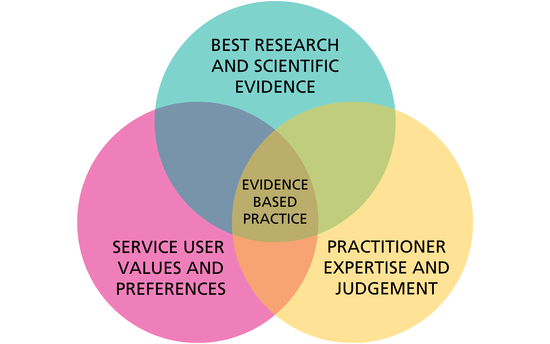
Evidence-Based Practice (EBP) requires that decisions about health care are based on the best available, current, valid and relevant evidence. These decisions should be made by those receiving care, informed by the tacit and explicit knowledge of those providing care, within the context of available resources.
Since 2005, there have been a variety of other statements, definitions and frameworks developed to outline EBP.
Within the field of nutrition and dietetics, a definition was first provided by the Academy of Nutrition and Dietetics (AND) in 2007. It was later defined by the International Conference of Dietetic Associations (ICDA) in 2010 as:
Asking questions, systematically finding research evidence, and assessing the validity, applicability and importance of that evidence. This evidence-based information is then combined with the dietitian’s expertise and judgment and the client’s or community’s unique values and circumstances to guide decision-making in dietetics to improve health outcomes in individual clients, communities and populations.
This 2010 definition from the ICDA, has been adopted by a number of other organisations including The European Federation of the Associations of Dietitians (EFAD), and subsequently by the BDA.
Benefits of evidence-based practice:
The benefits of implementing EBP are far reaching, and the evidence consistently demonstrates that this approach can:
- Improve the quality of healthcare
- Improve service user outcomes
- Reduce healthcare costs
- Contribute to the growth of the science of nutrition and dietetics
- Increase practitioner autonomy and confidence in decision making
- Guide research priorities
- Standardise practice
Useful Links
Resources