In this chapter:
- The process of menu planning
- Menu type
- Standard menu structure
- Menu content
- Other considerations
- Printed menu guidance
Catering and food services must be capable of providing food and drink suitable for all patients in their care. Patient needs and type of menu are two of the first considerations in menu design.
This chapter focuses on the process of planning a menu. It also looks at menu design and food-based guidance to create menus that meet the dietary needs of patients and the nutrition standards outlined in Chapter 10.
The process of menu planning
Menu planning requires a multidisciplinary approach – it should involve representatives from all key groups responsible for food provision, including catering, dietetics and nursing. This approach will ensure that all stakeholders are involved from the beginning and that all requirements are met.
Figure 9.1 provides an overview of the menu planning process and Table 9.1 goes into more detail for each step.
Throughout the whole process, there needs to be a focus on meal nutrition, taste and appeal to patients. While cost and logistics are important elements of menu planning, there is no nutritional or economic value in uneaten meals.
Figure 9.1 An overview of menu planning
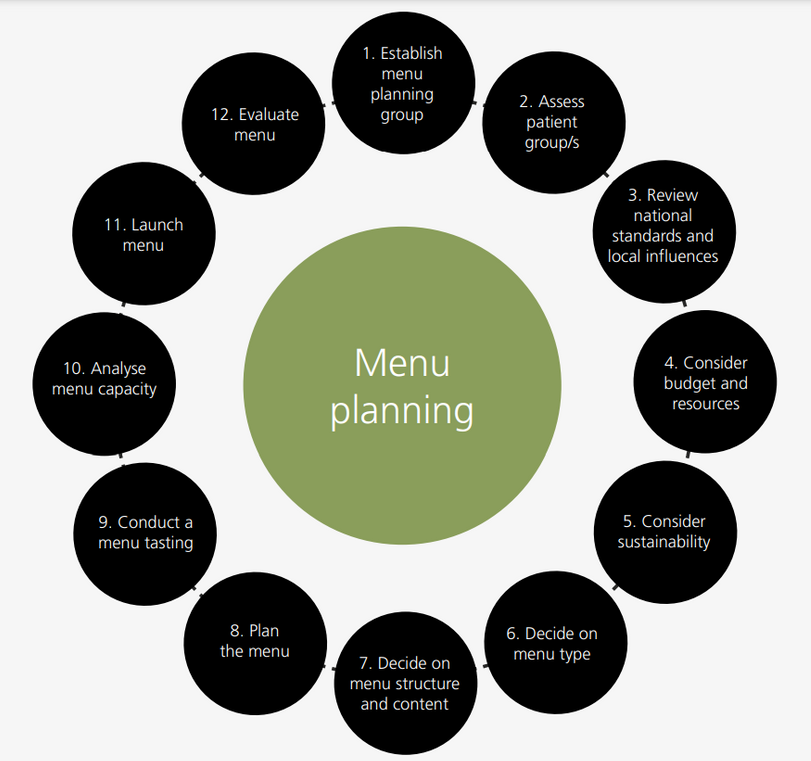
Table 9.1 The process of menu planning
|
The process of menu planning |
|
|---|---|
|
1. Establish menu planning group |
|
|
2. Assess patient group/s |
|
|
3. Review national standards and local influences |
|
|
4. Consider budget and resources |
|
|
5. Consider sustainability |
|
|
6. Decide on menu type
|
|
|
7. Decide on menu structure and content
|
|
|
8. Plan the menu
|
|
|
9. Conduct a menu tasting |
|
|
10. Analyse menu capacity |
|
|
11. Launch menu |
|
|
12. Evaluate menu |
|
Menu type
There are three main types of menus used in healthcare settings – cyclical, a la carte and hybrid. See Table 9.2 below for a description of each.
Table 9.2 Different menu types
|
Cyclical A menu with different meal options for the cycle period, typically 1 – 4 weeks. This type of menu provides a set number of choices for each meal service and the menu is repeated at the end of the cycle.
|
À la Carte A menu with an extended choice of defined meal options that remains the same every day.
|
|
Hybrid |
|
|
A menu that combines an a la carte menu and a cyclical menu. Within a meal service, it contains some options that are available every day and a cycle of some options that change each day (i.e., daily specials).
|
|
Some healthcare settings use more than one type of menu, e.g., maternity and A&E may offer an a la carte menu, while the rest of the hospital utilises a cyclical menu. The risk of menu fatigue should be considered when planning any menus and strategies for combatting this issue should be discussed in the early stages of menu planning.
Whichever approach is chosen, it is crucial that the menu design meets the dietary needs of those who will use it.
Standard menu structure
Menu structure refers to the overall types of food and drink, the number and variety of choices offered and at which times of the day. The structure will differ slightly depending on the menu type. It should be based on an eating pattern that is recognisable and compatible with the patient group it is designed for.
Breakfast offerings are similar across most healthcare settings, whether using a cyclical or an a la carte menu for main meals. At lunch and dinner, there should be a minimum of two courses offered to patients: a main meal and a dessert. Starters are optional. This ensures the two courses with the greatest nutritional value are available for nutritionally vulnerable patients who require more nutrient dense food.
The decision to serve either a two or three course meal should be based on the patient group being catered for. This must be discussed at the menu planning stage on a hospital-by-hospital basis to ensure the dietary needs for the population group are met.
A sample format for both a standard cyclical and à la carte menus is suggested below (Table 9.3). This does not include guidance for special menus. Further information about each course and dish type can be found in the next section that covers menu content.
Table 9.3 Standard menu structure
|
|
Standard menu structure |
||
|---|---|---|---|
|
Early morning |
Drink |
||
|
Breakfast |
Standard breakfast items (see menu content section below) Any special breakfast items for certain patient groups Drink |
||
|
Mid-morning |
Drink + snack |
||
|
|
Cyclical Menu |
À la carte menu |
|
|
Lunch & dinner |
Starter – optional Main meal Minimum 3 main entrées – one of which is vegetarian, + carbohydrate side (i.e., potato or grain based) + vegetable side (fresh or cooked) for each day of the cycle A range of salads (meat/fish/vegetarian) A range of sandwiches (meat/fish/vegetarian) Dessert Hot dessert + custard or milk pudding Cold dessert Drink |
Starter – optional Main meal Minimum 14 choices of hot main meals (to provide a different option at lunch and dinner for a one-week period), including: Article I: meat, fish or vegetarian based entrée + carbohydrate side (i.e., potato or grain based) + vegetable side (fresh or cooked) Article II: or composite dish that includes the main entrée, vegetables and/or potatoes/grains A range of salads (meat/fish/vegetarian) A range of sandwiches (meat/fish/vegetarian) Dessert Hot dessert + custard or milk pudding Cold dessert Drink |
|
|
Mid-afternoon |
Drink + / - snack |
||
|
Evening |
Drink + snack |
||
Exceptions to the standard menu structure
À la carte menus, such as those used for special and therapeutic diets, should strive to meet the above standards, but it is recognised that this may not always be possible with very restrictive diets e.g., low fibre, multiple allergies and texture modified. In these cases, specialist dietitians should be involved.
The type of meal provided, food storage and ordering procedures need to be carefully considered in these situations. Care should be taken to ensure that these menus are designed to provide an appropriate range of options relevant to the patient group, type of hospital and the length of stay and should be sufficient to avoid menu fatigue.
For patients who may be nutritionally vulnerable and for whom complete meal options may not be realistic, such as those recommended to follow a ‘little and often’ eating pattern, a grazing style menu should be encouraged.
Menu content
This section provides an overview of the recommended types of food and drink to include in a standard hospital menu to ensure that the nutrition standards, outlined in Chapter 10, can be met.
The Eatwell Guide
As a minimum and to ensure that requirements for protein, minerals and micronutrients are met, menus should be able to provide the following each day, as outlined by the Eatwell Guide in figure 9.2 (3):
- Fruit and vegetables (5 servings)
- Potatoes, bread, rice, pasta and starchy carbohydrates (5 servings).
- Dairy and alternatives (3 servings).
- Beans, pulses, fish, eggs, meat and other proteins (2 servings).
- Foods with a high fat or sugar content may be offered, but the emphasis will be different depending on individual needs. Choices which provide important nutrients should always be given priority. In the case of nutritionally vulnerable patients, nutrient dense options may also include added fat and sugar to make useful contributions to the overall requirements.
Figure 9.2: The Eatwell Guide
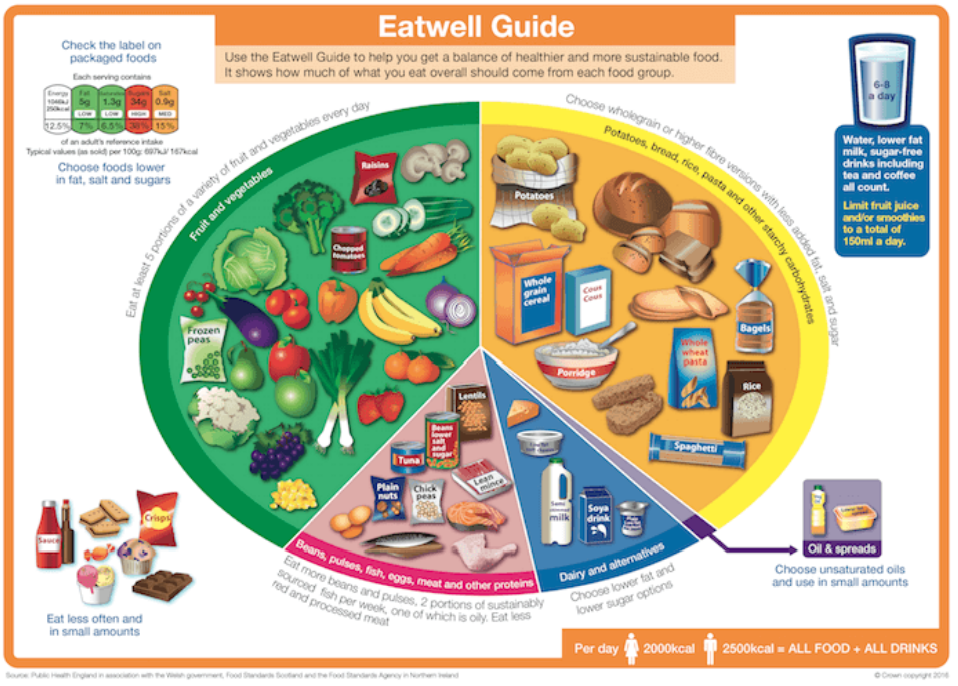
Eatwell Guide must be acknowledged as Crown copyright and the following statement included to identify the source: Public Health England in association with the Welsh government, Food Standards Scotland and the Food Standards Agency in Northern Ireland. https://www.gov.uk/government/publications/the-eatwell-guide
Breakfast
Breakfast may be provided at ward level using ward provisions or as a full meal service through the catering team. Regardless, there needs to be a clear process for the delivery of breakfast to patients and a consistent offer of choices, supported by a solid supply chain.
Breakfast generally consists of continental-style choices and as a minimum the daily standard breakfast should offer:
- Fruit juice: A range of juices, e.g., apple and orange juice. 85ml cuplets are often used in healthcare settings, however 150ml of unsweetened 100% fruit juice is equivalent to one portion of fruit. Regardless of whether more is consumed, fruit juice can only ever count as one portion of the ‘5-a-day’ target (3).
- Cereals with milk:
- A range of cold cereals – including both higher fibre options, e.g., branflakes, wheat biscuits, and lower fibre options, e.g. cornflakes, rice krispies
- At least one hot cereal choice, e.g. porridge or a smooth oat-based cereal
- A choice of full fat, semi-skimmed and a calcium fortified dairy alternative drink should be available to serve with the cereals.
- Bread/toast: White and wholemeal sliced bread or rolls. Where it is operationally feasible and where quality can be assured, toasted bread should be offered to patients. Patients may choose to have more than one slice of bread.
- Spreads: Both butter and a dairy alternative fat spread.
- Preserves: Assorted jam and marmalade. Other options, such as Marmite and honey are optional.
Depending on the patient group and facilities, additional higher protein breakfast items such as yoghurt, cooked breakfast items, fortified porridge or fortified milk, should also be offered to ensure requirements are met for nutritionally vulnerable patients.
Table 9.4 outlines the minimum breakfast assumptions, which provide adequate energy and protein for nutritionally well patients, as outlined in Chapter 10.
Table 9.4 Minimum breakfast assumptions
|
Breakfast item |
Minimum amount per patient |
|---|---|
|
Fruit juice |
1 serving (~85ml) |
|
Cereal |
1 serving (~30-40g) |
|
Milk |
100ml to be served with cereal |
|
Bread/toast |
1 slice (~40g) |
|
Spreads |
1 packet per slice of bread/toast (~6-10g) |
|
Preserves |
1 packet per slice of bread/toast (~20g) |
Lunch and dinner
Starters
Soup
As a starter, soup can be a good way to increase the vegetable intake of patients, but the portion size should be limited to roughly 150ml. This will help ensure that nutritionally vulnerable patients do not fill up on soup and as a result, not eat their main meal, which is higher in protein and other key nutrients. Soup can be a popular choice for unwell patients; however, a starter portion of soup should only be served before a main meal and not as a replacement.
Soup should only be provided as a starter if it meets the minimum nutritional criteria of a ‘nourishing soup’ as outlined in Chapter 10. Soups that are of poor nutritional quality (e.g., some whisk and serve style soups) should not be used in the healthcare setting. If a patient would like to have soup as their main meal, then larger portions of ‘fortified soup’ should be included in the mains section of the menu (see Main Meals section below).
Service times should factor in multiple courses to ensure food is served to patients at a safe (i.e., >63°C) and enjoyable temperature. This will look different for each hospital ward depending on the number of beds, levels of staffing, available equipment and the budget for extra ward support at mealtimes.
Other options
Alternative options could be offered as a starter if an item meets the clinical need of a patient group, and the menu continues to meet daily nutrition standards (outlined in Chapter 10).
Main meals
Hot main course
Standard hospital menus should provide an adequate choice of hot main meals that cater to both nutritionally well and nutritionally vulnerable patients. They should also include vegetarian options and options that are easy to chew (see Chapter 12) at each meal service.
Portion sizes for main courses or main meals are not set at any target. Dishes can have varying nutrient densities. For example, two different fruit crumbles may weigh the same or visually look the same size on a plate, but one may have a significantly higher fruit to crumble ratio than the other. Less focus should be placed on the weight of main meal portions and more priority placed on the nutrition content. See Chapter 10 for more information on nutrition standards.
Carbohydrate sides
At least one carbohydrate-based side dish should be offered as part of a hot main course. This could be potatoes, rice, pasta, bread or other grain options like cous cous, pearl barley or quinoa.
The type of side dishes offered should reflect the needs and preferences of the patient group. For example, if there is a high proportion of older adults, at least one easy to chew side, such as mashed potato, should be offered at each meal service. The side dishes should also compliment the main entrees they are served with, e.g., rice with a vegetable curry or roast potatoes with roast chicken.
Vegetable sides
When choosing vegetable options for a main course, the following should be considered:
- Minimum portion size of a vegetable serving is 80g per meal.
- Consider serving two different vegetables per meal to increase variety and choice.
- Using vegetables of different colours and textures in a meal service creates more appealing meals.
- Ensure at least one of the vegetables at each meal service is coded as an easy to chew option (as defined in Chapter 12).
- Popular choices and seasonal vegetables should be routinely planned, when possible.
- Higher protein vegetables, such as peas and baked beans can be offered with lower protein entrees to improve the overall meal protein content.
Sauces, condiments, garnishes and gravy
Sauces, condiments, garnishes and gravy could also be considered to complement and improve the overall palatability of a meal, such as offering a slice of lemon and tartare sauce with fish and chips or offering natural yoghurt with a curry dish.
Food costs and sustainability issues, such as increasing food waste should be considered carefully. It is also important to be aware that some people do not like sauces, therefore plainer meals without sauce should also be offered. To cater to different preferences, it is best to implement ordering and meal service systems that allow for choice.
Main meal soup
Soups as main meal option can be appealing for patients with a poor appetite or who are feeling generally unwell. A main meal soup should be a larger portion than a starter soup. The soup itself also needs to meet the minimum nutrition criteria of a ‘fortified soup’ and be served with suitable accompaniments (e.g., bread roll and spread) to ensure it meets the minimum nutrition criteria for a main meal. Both the minimum energy and protein criteria for a fortified soup and a main meal are outlined in Chapter 10.
Sandwiches
Sandwiches may be offered to patients as an alternative to a hot main meal.
The minimum nutrition criteria for sandwiches served as a main meal option is outlined in Chapter 10. Sandwiches also need to be able to provide the same minimum nutrition targets for a complete main meal (i.e., with a dessert and where applicable, a starter). To meet these targets, sandwich options may require the addition of a side dish, such as coleslaw, other salads, crisps or chips to increase the overall nutritional value.
A selection of sandwiches should be available to meet the different dietary needs of patients, including easy to chew, healthier eating, higher energy and vegetarian options. It is best practice to offer sandwiches that cater to other special diets, such as Gluten Free, Halal and Vegan, however, the selection of sandwiches and order volumes will be dependent on the requirements of patients for each individual healthcare facility. It is also important to consider uptake volumes to avoid food waste.
When choosing the types of sandwiches to offer, ensure there is a choice of white and wholemeal bread available and opt for fillings and types of bread that are more popular and nutritious.
Sandwiches such as plain ham, chicken or cheese may be required as a flexible component to the food offer for different patient groups, such as children, those requiring special diets, such as low fibre and those with food allergies.
Accessible design of packaging for sandwiches should be considered in line with the requirements set out in Chapter 6.
A note on soup and sandwich meals
While soup and sandwich options are fine to offer on a standard menu, a soup and sandwich meal must not be the only main meal choice available at a given meal service due to the inability of this option to meet the higher nutrition requirements of nutritionally vulnerable patients (4). An alternative option must always be available.
Salads
A salad meal is a welcome addition to a menu, especially in summer months.
The minimum nutrition criteria for a salad served as a main meal is outlined in Chapter 10. As with sandwiches, main meal salads also need to be able to provide the minimum nutrition targets for a complete main meal. To ensure nutrition targets can be met, a salad should contain a good source of protein and either be served with or contain a source of carbohydrates, such as pasta, potato, a bread roll, rice or other grains.
Desserts
Some desserts can contribute a significant number of calories and enjoyment to a menu, which is especially important for nutritionally vulnerable patients. Menus should include at least one higher energy, and ideally higher protein, dessert option at each meal service to cater for nutritionally vulnerable patients. See Chapter 12 for the nutrition criteria of a higher energy dessert. These desserts may include fruit crumble, sponge with chocolate or jam, puddings or cheese and crackers. They can also be served with custard or ice cream to increase their overall energy and protein content.
Menus should also offer healthier eating dessert choices, including fresh or tinned fruit, custard and yoghurt.
Snacks
A minimum of two different types of snacks should be offered to patients twice a day to support additional nutritional requirements. Snacks should be provided at either mid-morning or mid-afternoon and in the evening.
The range of snacks should include both healthier eating and higher energy options to cater for both nutritionally well and nutritionally vulnerable patients. The minimum nutrition targets for snacks for both groups are outlined in the day parts approach (Table 10.4) in Chapter 10. Refer to Chapter 12 for the menu coding of individual snacks.
Healthier eating choices may include fruit, yoghurt, crackers or wholegrain crispbreads. While higher energy options could include muffins, cakes, flapjacks or cheese and crackers. Higher protein snacks should also be considered to meet the needs of nutritionally vulnerable patients.
It is important to offer a selection of snacks that also cater to different dietary needs, such as vegetarian, vegan, easy to chew, gluten free, modified texture and culturally appropriate options, and to different patient groups, such as children and older adults (4).
Drinks
The Healthcare Caterers Association (HCA) Good Practice Guide (5) recommends offering seven drinks over the day as a minimum. In addition to tea and coffee, other drinks like squash, milk-based hot drinks and fresh water must also be readily available. Options should also include decaffeinated tea and coffee and consideration should be given to the provision of fruit juice, fruit teas or malted milk drinks.
The choices of drinks available should reflect the needs of the patients being served. For example, a children’s ward may not offer caffeinated drinks or certain renal wards may choose to avoid serving chocolate-based drinks.
- 400ml of milk as a minimum should be allocated per patient for drinks.
This excludes milk for breakfast, where a minimum of 100ml should be allocated. Where patients are nutritionally vulnerable, whole milk should be provided as standard. Children under the age of 2 years old should not be given skimmed or semi skimmed milk. A dairy free drink, fortified with calcium, should always be available as an alternative to cow’s milk, e.g. soya or oat based drinks supplied for vegan or patients with a cow’s milk protein allergy or intolerance.
Other considerations
24-hour meal provision
Patients should have access to suitable 24/7 food and drink options, which are appropriate for their demographic (6) and dietary needs (4). This includes patients with any special dietary needs, including cultural, allergen free and modified texture.
Meals served outside of the dedicated meal service times should provide a choice for all patient groups and be capable of providing the same minimum nutrition as a main meal, as outlined in Chapter 10.
The process for ordering meals outside of regular meal service times should be clear and well communicated throughout the facility to ensure patients who have missed a meal can meet their nutrition needs. It is also critical that any staff providing ‘out of hours’ hot meals have completed the appropriate food safety training and that meals service records are kept.
Alcohol as a recipe ingredient
While alcohol as an ingredient can enrich the flavour of a dish and most of the alcohol content is evaporated during cooking processes, there are some considerations to make when alcohol is used in recipes for healthcare settings.
To ensure that the needs of all people are met, it is good practice to always include the alcohol ingredient in the dish name, e.g. steak and ale pie, so that there is no uncertainty about whether or not alcohol has been included as a dish ingredient. It provides transparency for people who avoid alcohol for clinical, cultural or religious reasons and enables hospitals that have an alcohol-free policy to confidently plan menus that do not contain any alcohol.
Vitamin analysis
Dietitians and other members of the menu planning team may wish to gain assurance that all nutritional targets are met, including vitamin and minerals. Reference intakes of individual nutrients for the well population can be found on the British Nutrition Website (7) and within The Eatwell Guide from Public Health England (8).
Menu checklist
The menu planner should assess the food-based standards outlined in this chapter by using the Qualitative Menu Assessment Checklist provided in Appendix 1.
This tool can be adapted to reflect the needs of the patient groups served where some elements may not be applicable or appropriate.
Printed menu guidance
Patients should be provided with printed menu information to allow them to consider their food and drink choices and assist with the meal ordering process. There are several print menu designs now being used within healthcare settings – e.g. menu booklet, poster, tray mat, menu slips or cards. It is important to consider the sustainability aspects of a printed menu. Where less paper is used there is an ultimate saving in the greenhouse gas emissions associated with paper.
Consideration should be made as to which design best communicates information to patients to help them decide what to order. The table below lists the most important information or signposting that is typically displayed on healthcare menus. It is also important to consider legibility and accessibility of the menu design and the budget for printing menus.
Table 9.4 Information and guidance on printed menus
|
Importance of nutrition & hydration whilst in hospital |
|
Signposting to allergen (legally required) and nutritional information |
|
Menu coding descriptions |
|
Meal service times and missed meal procedure (24/7 food service options) |
|
Other menus available e.g. special diet menus, pictorial menus |
|
Patient satisfaction survey link or instructions for providing feedback |
|
Assisted or protected mealtimes information |
|
Sustainability information |
|
Breakfast, lunch, dinner, snack and drink options |
|
Meal ordering instructions |
Click here to go to the next chapter.
Click here to return to the top of the page.
References
- NHS England and C4PC (2020) A co-production model. https://coalitionforpersonalisedcare.org.uk/resources/a-co-production-model/ [Accessed 2nd April 2023]
- Bowen L et al. Food service in hospitals and institutions. In: Gandy J. (ed.) Manual of Dietetic Practice. 6th ed. UK. Wiley Blackwell on behalf of The British Dietetic Association; 2019. p. 260-270.
- Public Health England. The Eatwell Guide: The Eatwell Guide Booklet. 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/742750/Eatwell_Guide_booklet_2018v4.pdf [Accessed 2nd April 2023]
- Department of Health and Social Care. Report of the Independent review of NHS hospital food. 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/929234/independent-review-of-nhs-hospital-food-report.pdf [Accessed 2nd April 2023]
- Hospital Caterers Association. A Good Practice Guide to ward level services. Healthcare Food and Beverage Service Standards. Manchester: Lansdowne Publishing Partnership Limited; 2013. http://www.hospitalcaterers.org/publications/ [Accessed 2nd April 2023]
- NHS England. National standards for healthcare food and drink. 2022. https://www.england.nhs.uk/publication/national-standards-for-healthcare-food-and-drink/ [Accessed 2nd April 2023]
- British Nutrition Foundation. Vitamins and minerals in a healthy Diet. https://www.nutrition.org.uk/healthy-sustainable-diets/vitamins-and-minerals/?level=Consumer [Accessed 2nd April 2023]
- Public Health England. Government Dietary Recommendations: Government recommendations for energy and nutrients for males and females ages 1-18 and 19+ years. London: Public Health England; 2016. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/618167/government_dietary_recommendations.pdf [Accessed 2nd April 2023]

