In this chapter:
We need to work together to combat climate change. By making dietary changes, it’s win-win for the planet and health if we all act now.
British Dietetic Association One Blue Dot
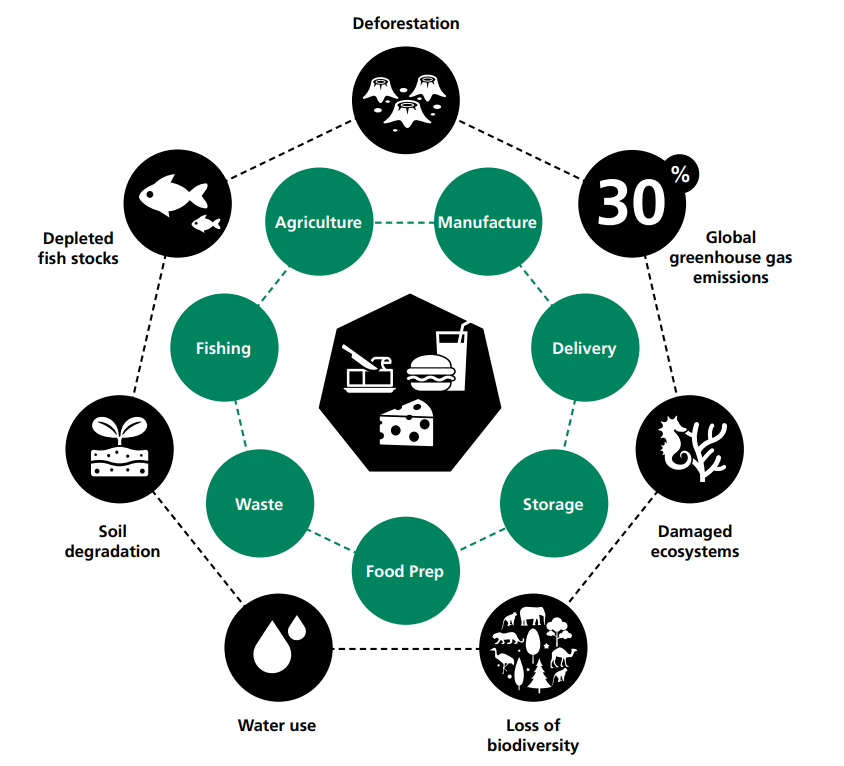
This chapter provides an overview of sustainability, the role of the multidisciplinary team and some practical guidance for hospital food service to make impactful changes. Climate change threatens the foundations of good health, with direct and immediate consequences for our patients and the public. Our eating habits have an impact on the environment and are jeopardising the future security of our planet including farming, production, distribution and delivery through to waste (1).
The impact of food systems on the planet
Our current food system is having a major negative impact on our planet. This impact is summarised by the below statistics and Figure 4.1 from BDA's One Blue Dot.
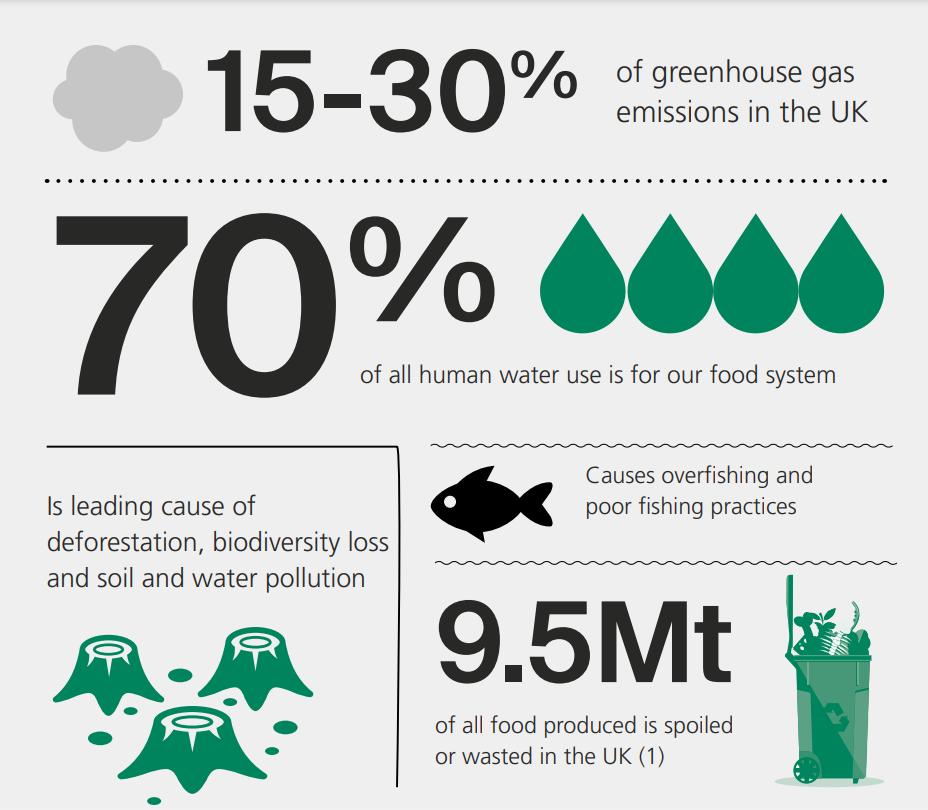
Figure 4.1: How current food systems damage our planet - BDA One Blue Dot (1)
In the UK, approximately 46% percent of the food we eat is imported from other countries (2). The transport of food from abroad increases the environmental impact of our food system, plus there is an increased risk of spoilage and food waste en route.
A more sustainable way forward
Research on sustainability is fast paced and more sustainable practices are emerging. There are now a number of new ways to grow food, including hydroponics and 'no ploughing' farming practices. Similarly, waste disposal methods now range from traditional landfill to innovative practices like incineration for heat provision and bio-digesters.
There has also been advancement in the nutrition advice for sustainable eating patterns in both the general population and for those who follow a specific diet for a clinical condition (1, 3, 4). Dietitians are well placed to apply knowledge of sustainable diets appropriately to their area of practice.
Sustainability in healthcare food service
Over the last 10 years, the National Health Service (NHS) has taken notable steps to reduce its impact on climate change. The Independent Review of Hospital Food conducted in 2020 recommends that sustainability is considered in all aspects of healthcare food service due to the environmental impact of the whole food supply chain, including procurement and waste (5).
The NHS has committed to reaching net zero carbon by 2040 for the emissions it controls directly (i.e. Scope 1) and by 2045 for the emissions it influences. The goods and services purchased by the NHS are part of the indirect category, known as Scope 3. As outlined in Figure 4.2, food and catering are included in Scope 3 of the Greenhouse Gas Protocol (GHGP) (6).
Figure 4.2: GHGP (Greenhouse Gas Protocol) scopes in the context of the NHS (6)
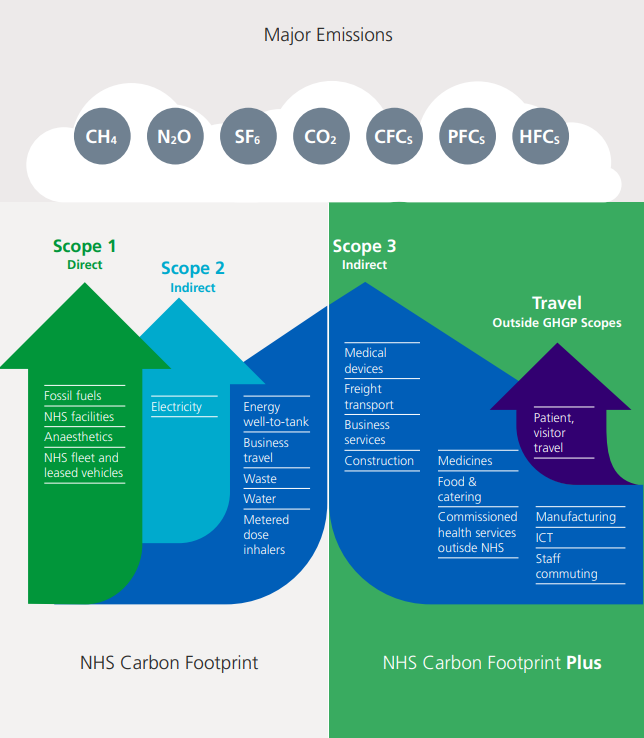
It is estimated that food and catering services in the NHS produce 1,543 ktCO2e each year, equating to approximately 6% of total emissions. In some cases, locally sourced food can cut emissions related to agriculture, transport, storage and waste across the supply chain and on the NHS estate (6).
To reduce the impact of it’s supply chain, the NHS has set out a roadmap to help suppliers align with its net zero ambition between now and 2030. This includes the requirement from April 2022 that all NHS procurements apply a minimum 10% net zero and social value weighting in the award of NHS contracts. Also, from April 2023 there will be a requirement for all suppliers of contracts over £5m to publish a carbon reduction plan. Full details of these and other requirements can be seen in the net zero supplier roadmap (7).
Every NHS Trust and Integrated Care System (ICS) is required to develop a board-approved Green Plan that sets out their aims, objectives, and delivery plans for carbon reduction, with a board-level ‘net zero lead’ responsible for overseeing its delivery. These plans should set out how trusts are reducing the carbon emissions from any food made, processed or served within the organisation (8).
The National standards for healthcare food and drink
The National standards for healthcare food and drink include a whole section on sustainability (9). It is mandatory for all healthcare organisations in England to comply with section 4 of the standards, titled ‘Improving sustainable procurement and reducing food waste’. The section covers compliance with the Government Buying Standards for Food and Catering Services, food procurement practices in line with the Net Zero and Social Value Model, measuring and reducing food waste and the elimination of single use plastics. See Chapter 3 for more information on the National standards for Healthcare Food and Drink.
Environmentally sustainable diets
The British Dietetic Association (BDA) has published an extensive policy statement on the topic of environmentally sustainable diets. Titled ‘One Blue Dot’ (1), the policy statement and toolkit supports the belief that “everyone should have access to an affordable nutritious, high-quality diet that is good both for health and the environment”.
The aim is to ensure that UK dietitians lead on dietary changes and nutritional considerations. The BDA’s Sustainable Diets Specialist Group has also been established to help support dietitians and work with other organisations (10).
Plant based diets
The BDA describes plant-based diets as ‘based on foods that come from plants with few or no ingredients that come from animals’ (11). There is increasing recognisition that plant-based diets have a lower impact on the environment, which doesn’t necessarily include the exclusion of meat, rather smaller quantities of animal derived foods. The UK Committee on Climate Change have discussed targets such as 20% less meat (12), while the Eating Better Alliance is calling for a 50% reduction in meat and dairy consumption (13).
It is possible to meet nutrient requirements with a diet that has less or no meat. The Scientific Advisory Committee on Nutrition (SACN) have advised that reducing the red meat intakes of adults who currently consume red meat in the upper range, down to 80g/day, would have little impact on the proportion of adults with zinc and iron intakes below the lower nutrient reference value (14).
The Eatwell Guide
The Eatwell Guide is the national food guide and recommends that the majority of the overall diet should be made up of plants i.e., fruits, vegetables, grains and legumes (15). See Chapter 9 for more on the Eatwell Guide recommendations.
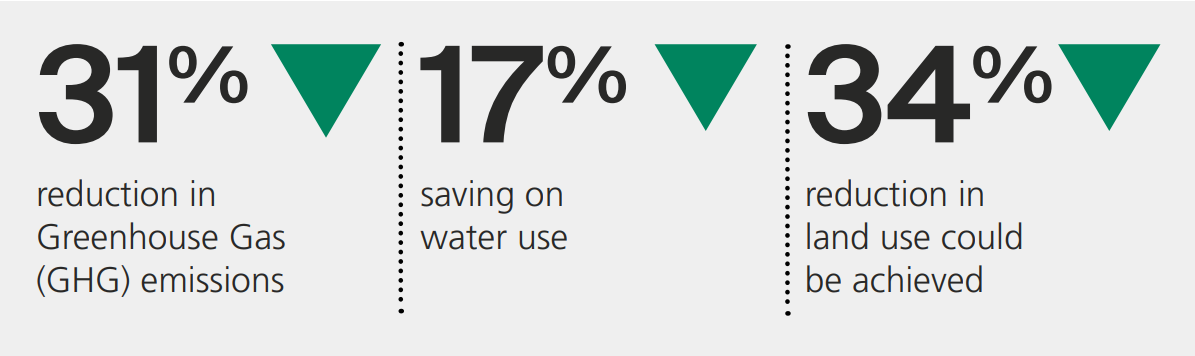
The Carbon Trust analysis of the Eatwell Guide shows that this diet has a lower environmental impact than the current UK diet attributed to several factors, including an increase in potatoes, fish, bread, vegetables and fruit, alongside reduced amounts of meat, dairy and sweet foods (16). The Carbon Trust estimates that if individuals moved from current eating patterns to the Eatwell Guide recommendations this would result in (16):
Lower carbon menus
Plant based proteins have been found to produce far fewer carbon emissions in their production than animal-based proteins (17). Including a good variety of plant-based dishes and reducing the availability of dishes with a higher carbon cost, such as red meat dishes, is a good way to help lower the carbon footprint of healthcare menus (1). However, it is important that plant-based dishes still meet the minimum nutrition targets outlined in Chapter 10, so patients can meet their daily nutrition requirements.
Plant-based dishes must also be appealing, to encourage patients to choose these options and eat the whole meal to gain it’s full nutritional value. There are several methods to help nudge patients to choose plant-based options (18). These include:
- Use positive language such as ‘plant-based protein’ and avoiding using the terms ‘vegetarian’ and ‘vegan’ in the name of dishes so that they appeal to a wider audience.
- Position plant-based options at the start of menus to increase the likelihood that they are seen by patients as they read down the list of options.
Carbon labelling is also a new tool to help signpost people to lower carbon/more environmentally friendly food choices. The carbon label may be a numeric CO2 emission value or a rating system so that people can compare dishes based on their carbon footprint. The calculations consider the amount of carbon produced during the farming and transport of each ingredient and the production of the complete dish.
Once carbon emissions of ingredients are known, chefs and dietitians could also use these values when developing recipes to choose lower carbon ingredients to reduce the overall carbon footprint of the menu. Whilst software programs are available to calculate the carbon footprint of food, recipes and menus, they are in their infancy and results are often variable.
Nutrition is the key priority for patient menus, so annotating carbon labelling directly on patient menus may be inappropriate.
Comparisons between products can also only be made if the same methodology for calculating the carbon footprint has been used. Therefore, if ratings are provided by different suppliers who use different methods, these products cannot be directly compared (19). While carbon labelling may become mandatory for retailers in the future, guidelines are yet to be agreed as to what should be measured and how. Free online calculators are available; however, these may be misleading, as they utilise generic datasets and do not give specific values for the actual ingredients used.
Industry stakeholders are working on a common set of data sources and consistent methodology for measuring and verifying emissions of food and drink products, which is essential for any on-pack carbon labelling (20).
Role of the multidisciplinary team in sustainability
All members of the multidisciplinary team with a role in food service, including Allied Health Professionals (AHPs), interact with the food system in various ways and have a unique opportunity to be agents for change. See ‘further reading’ for the Greener AHP hub (21), which has specific considerations for food and nutrition. Potential actions that this team can take are outlined below:
- Individual Actions: Small everyday actions that together will have a significant net effect by embedding public health and prevention (and therefore environmental sustainability) in existing interventions e.g., through Making Every Contact Count (22).
- Waste: Seek an active role in reducing food and plate waste by including supporting “assisted mealtimes” and digital ordering (23). Resources are available to help reduce waste generated during both meal production and service (24). For example, meals cooked and served when a patient is Nil by Mouth or is off the ward, leads to the meal being wasted. It is also vital patient food preferences are communicated at ward level to reduce the risk of plate waste.
- Procurement: Those involved in procurement teams should review contracts for food, equipment and related items, aiming to achieve health and social benefits, financial savings and environmental benefits.
- Audits: Hospitals are required to carry out audits and include them at senior board level. While these have a focus on clinical, financial and operational issues, there is a requirement for an examination of maintenance of any standards including those related to sustainability.
Dietitians should be aware of the challenges for vulnerable groups and individuals (e.g., those suffering from ill health, pregnant women and older adults) and be able to modify advice as appropriate. This is never more important than dealing with ill and vulnerable people in hospital and care situations where a move to a totally plant based diet may be inappropriate.
Practical guidance
These best practice ideas, while not all mandatory, are useful pointers towards making the food, service and environment in healthcare more sustainable.
- Include more home-grown seasonal products on menus that are tailored to the preferences of local people and that can be provided safely and consistently
- Where appropriate, approach local suppliers to supply the hospital. Larger, national companies may rely more on UK produce where national supply contracts cannot always be ‘local’
- Consider introducing a logo on the menu to indicate that UK or local sourcing has been utilised
- Introduce meat-free menu options and initiatives such as Meat Free Mondays in staff and visitor restaurants
- Reduce the amount of meat in popular recipes like Spaghetti Bolognese by incorporating beans, legumes and other meat alternatives to help reduce the carbon footprint by as much 50%
- Utilise more sustainable options for printed menus for patients, such as large single page menus rather than multi-page booklets and menu displays for staff and visitor catering, such as digital menus or reusable menu boards
- Establish a procedure to consistently measure and monitor food waste at both kitchen and ward level
- Aim to recycle or convert food waste to fuel with bio-digesters or other commercial waste systems
- Utilise electronic or digital meal ordering systems and take patient meal orders as close to mealtimes as possible to help reduce food waste
- Appropriately recycle any food or drink packaging and limit any unnecessary packaging
- Use crockery and cutlery that can be reused instead of single use plastics. Where this is not possible, use biodegradable packaging which may be more sustainable.
- Decant bulk food and drink items where possible rather than use individually packaged items, unless clinically indicated
- Consider using circular recyling systems for unavoidable use of plastic packaging
- Consider introducing an initiative where reuseable cups or containers can be used in staff and visitor restaurants and coffee shops for a discount
- Educate staff about the environmental impact of more sustainable diets and where they may/may not be appropriate for certain patients
Click here to go to the next chapter.
Click here to return to the top of the page.
References
- British Dietetic Association. One Blue Dot: Eating patterns for health and environmental sustainability. https://www.bda.uk.com/resource/one-blue-dot.html [Accessed 11th April 2023]
- International Trade Administraion. United Kingdom – Country Commercial Guide. https://www.trade.gov/country-commercial-guides/united-kingdom-agricultural-sectors#:~:text=The%20UK%20imports%20around%2046,importer%2C%20especially%20of%20fresh%20produce [Accessed 11th April 2023]
- EAT. EAT-Lancet Commission Summary Report. https://eatforum.org/eat-lancet-commission/eat-lancet-commission-summary-report/ [Accessed 11th April 2023]
- Kassam S, Kassam Z, Simon L. Plant-based Nutrition in Clinical Practice. London. Hammersmith Books; 2022.
- Department of Health and Social Care. Report of the Independent Review of NHS Hospital Food. https://www.gov.uk/government/publications/independent-review-of-nhs-hospital-food [Accessed 11th April 2023]
- NHS England. Delivering a ‘Net Zero’ National Health Service. https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf [Accessed 11th April 2023]
- NHS England. Suppliers. https://www.england.nhs.uk/greenernhs/get-involved/suppliers/ [Accessed 11th April 2023]
- NHS England. How to produce a Green Plan: A three-year strategy towards net zero. https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2021/06/B0507-how-to-produce-a-green-plan-three-year-strategy-towards-net-zero-june-2021.pdf [Accessed 11th April 2023]
- NHS England. National standards for healthcare food and drink. https://www.england.nhs.uk/publication/national-standards-for-healthcare-food-and-drink/ [Accessed 11th April 2023]
- British Dietetic Association. Sustainable Diets Specialist Group. https://www.bda.uk.com/specialist-groups-and-branches/sustainable-diets-specialist-group.html [Accessed 11th April 2023]
- British Dietetic Association. Vegetarian, vegan and plant-based diet: Food Fact Sheet. https://www.bda.uk.com/resource/vegetarian-vegan-plant-based-diet.html [Accessed 11th April 2023]
- Climate Change Committee. Government’s Food Strategy ‘a missed opportunity’ for the climate. https://www.theccc.org.uk/2022/06/13/governments-food-strategy-a-missed-opportunity-for-the-climate/ [Accessed 11th April 2023]
- Eating Better alliance. Food Service. https://eating-better.org/better-by-half/food-service/ [Accessed 11th April 2023]
- Scientific Advisory Committee on Nutrition (SACN). Iron and Health. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/339309/SACN_Iron_and_Health_Report.pdf [Accessed 11th April 2023]
- Public Health England. The Eatwell Guide. https://www.gov.uk/government/publications/the-eatwell-guide [Accessed 11th April 2023]
- Carbon Trust. The eatwell guide: a more sustainable diet. https://www.carbontrust.com/our-work-and-impact/guides-reports-and-tools/the-eatwell-guide-a-more-sustainable-diet [Accessed 11th April 2023]
- Our World in Data. Greenhouse gas emissions per kilogram of food product. https://ourworldindata.org/grapher/ghg-per-kg-poore [Accessed 11th April 2023]
- Eating Better. Make plant dishes appealing. https://eating-better.org/better-by-half/food-service/make-plant-dishes-appealing/ [Accessed 11th April 2023]
- Our World in Data. You want to reduce the carbon footprint of your food? Focus on what you eat, not whether your food is local. https://ourworldindata.org/food-choice-vs-eating-local [Accessed 11th April 2023]
- Food and Drink Federation. Achieving Net Zero: A Handbook for the Food and Drink Sector. https://www.fdf.org.uk/fdf/resources/publications/guidance/net-zero-roadmap/net-zero-handbook/ [Accessed 11th April 2023]
- NHS England. Being a greener AHP. https://www.england.nhs.uk/ahp/greener-ahp-hub/understanding-environmental-sustainability/being-a-green-ahp/ [Accessed 11th April 2023]
- Public Health England, NHS England and Health Education England. Making Every Contact Count (MECC): Consensus statement. https://www.england.nhs.uk/wp-content/uploads/2016/04/making-every-contact-count.pdf [Accessed 11th April 2023]
- Young A. Protected Mealtimes (or Assisted Mealtimes?). https://dietitianconnection.com/app/uploads/2014/05/FS-workshop-assisted-mealtimes.pdf [Accessed 11th April 2023]
- Waste and Resources Action Programme (WRAP). Guardians of Grub. https://guardiansofgrub.com/ [Accessed 11th April 2023]
Further Reading
Public Sector Catering. Plant Based Week. https://www.publicsectorcatering.co.uk/plantbasedweek [Accessed 11th April 2023]
International Confederation of Dietetic Associations (ICDA). ICDA Sustainable Food Systems Toolkit. https://icdasustainability.org/?dm_i=1M7S%2C8047H%2C9LQ00X%2CWRP5D%2C1 [Accessed 11th April 2023]
Koutrouli, E. Identifying the challenges UK dietitians experience in implementing a food sustainability policy in the hospital setting. Unpublished Master’s thesis. The University of Manchester; 2021.

