The advanced level of practice is characterised by a high degree of autonomy, working in a multi-professional sphere, and the ability to manage complex decisions and risks in a dynamic environment. It is underpinned by post-registration Master’s level education (or equivalent) applied in practice. Advanced level practitioners independently manage entire services or pathways ensuring high quality, compassionate and inclusive care and leadership.
What is advanced level practice?
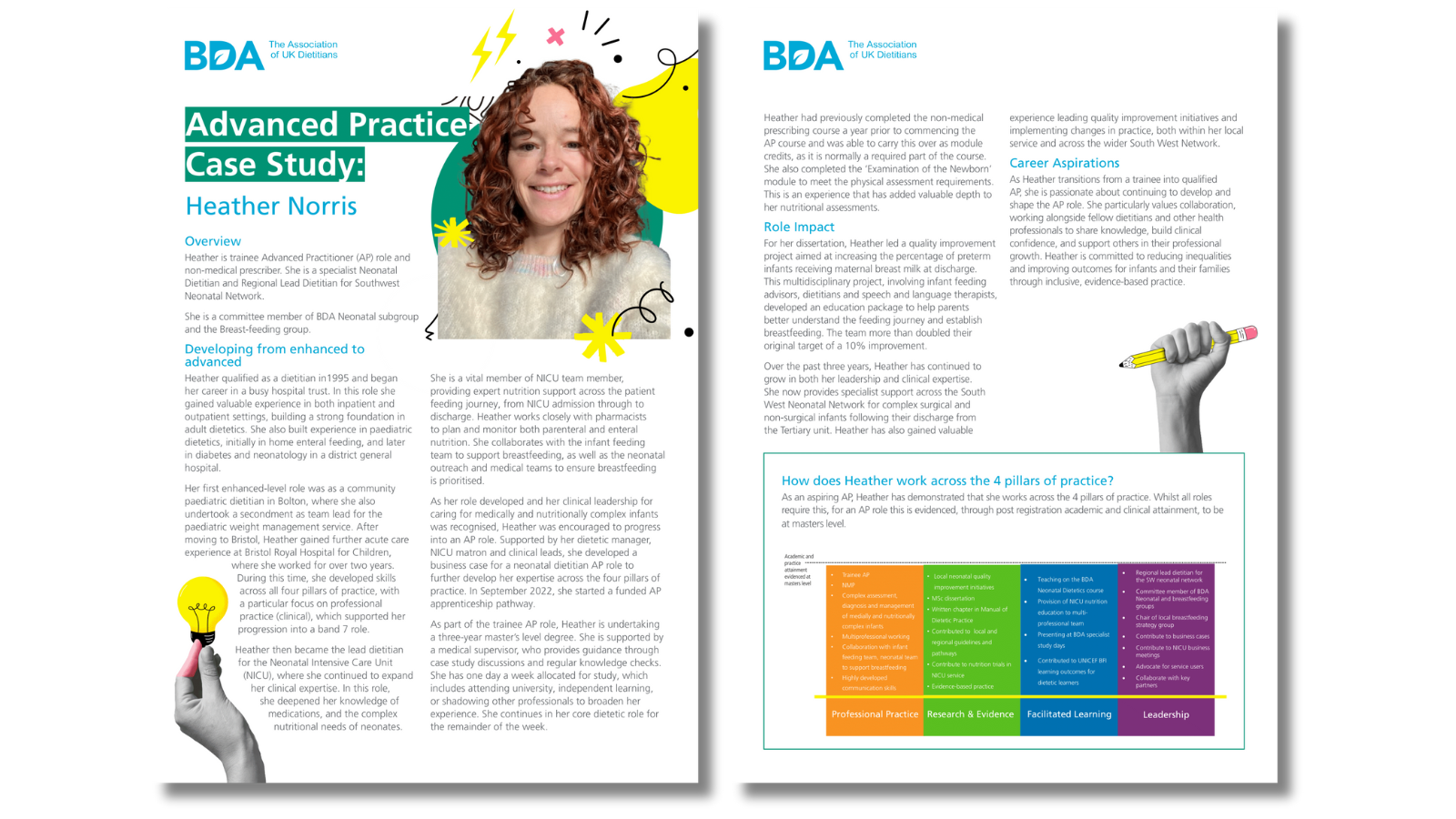
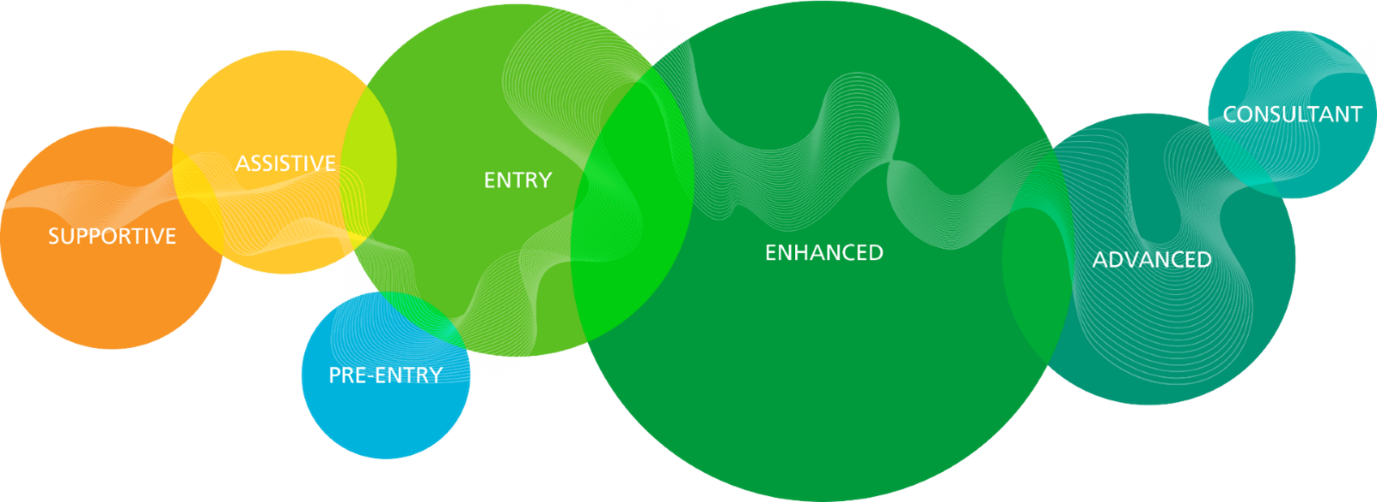
Advanced level practice is positioned between enhanced and consultant level practice. Only a small proportion of the workforce will be working at this level of practice, most of the registered workforce work at an enhanced level for their full career. Advanced level practitioners often work as part of the wider multi-professional team across professional boundaries with a broad sphere of influence outside of dietetics.
Roles and titles
Advanced level practice takes place in a wide range of settings and as such there will be many job titles and roles within this level. One example role is the ‘Advanced Practitioner’ previously referred to as an ‘Advanced Clinical Practitioner’ which is a clinical role deployed within the NHS in England. Whilst not everyone working at an advanced level will be in an advanced practitioner role, those using the title ‘Advanced Practitioner’ would be expected to map to the capabilities within the multi-professional framework for advanced practice in England and the BDA Dietetic Career Framework.
Examples of advanced level roles can be seen in our case studies.
Education and experience
Advanced level practice is developed through post registration education at Master’s level which is then applied in practice. This means demonstrating an ability to practice autonomously at a high level (Master’s level) across all four pillars of practice.
Many dietitians demonstrate their ability to achieve master’s level academic attainment through completion of a Master’s award at pre-registration level. At this point, however, they will be practising as a novice at the entry level of practice. Advanced level practitioners are experienced in their profession and will have completed post registration Master’s level education applicable to their specialist area. This education is likely to be multi, rather than uni-professional, as learning at this level usually requires a wider lens than your own professional scope.
Examples could include:
- Advanced Practice Master's (England)
- Master’s in Leadership & Management
- Master’s in Diabetes
- Advanced Clinical Practice (Critical Care)
- Master of Research (MRes)
- Postgraduate Certificate in Education
To develop professional capability, a commitment to lifelong learning is essential. Further information on the education requirements for advanced level practice is available by accessing the Dietetic Career Framework.
Accessing education and training
All members of the dietetic workforce have a responsibility at all stages of their career to keep their knowledge and skills up to date and to ensure they hold the relevant education and training to fulfil their role. This is essential to ensure you always work within your scope of practice.
However, we recognise that our workforce is experiencing challenges in accessing training opportunities which can result in recruitment and retention issues. Our ‘accessing education and training’ webpage has been developed with relevant and useful information to support you to access and engage in education and training.

Training and education opportunities across the four nations
Within the NHS England Long Term Workforce Plan (2023) there is recognition and a commitment to invest in funded and sustainable training pathways to support career progression for AHPs and to retain staff within NHS settings. This includes:
- All AHPs working in the NHS in England have access to funding for CPD through their employing organisation. As of 2025, this funding equates to £333 per year. Ask your line manager or Trust education lead for more information on this.
- NHSE Centre for Advancing Practice has access to funding for advanced level education including advanced practice masters. There is also an option, through a supported e-portfolio route, to enable recognition with the Centre of your existing role. This is aimed at experienced practitioners working in ‘Advanced Practitioner’ roles who completed their experiential and educational learning before the Centre existed.
- Many higher education institutes (HEIs) across England have access to multi-professional Master’s level education but not all courses will be the same. Do your own research to find a course that best suits your education and career aspirations.
Developing advanced level roles
The growth and development of the existing workforce is crucial in meeting current and future population healthcare needs. Service users are living longer with multi-morbidity meaning pathways of care are becoming increasingly complex.
For this reason, there is a clear need for highly experienced registered health and care professionals to be trained and deployed at an advanced level of practice. Whilst many roles at this level already exist, the BDA is keen to support members to look for opportunities to develop new roles to enable workforce transformation. There are many pathways whereby having advanced practitioners with a dietetic background could significantly improve the outcomes and experience for service users.
A simple step-by-step guide below aims to help members navigate the process of developing new roles. The process is likely to be more complex than this guide suggests and will vary in each organisation.
|
1. Identify the opportunity |
Work with stakeholders to identify a gap or need within the service or population. For example, a multidisciplinary pathway that requires significant nutrition and dietetic interventions. Could upskilling a member of the team reduce the input needed from other members of the MDT which would make the pathway more efficient? Be aware that the multi-professional nature of advanced level practice means that a dietitian may not be the only potential profession that could fulfil the role. |
|
2. Sell the opportunity to decision-makers |
Develop a business case that articulates the opportunity an advanced practice role brings to the pathway. This should include cost efficiencies, potential health outcomes, and improving access to address health inequalities. Organisations should have business case templates for this purpose. An example is provided here. |
|
3. Advertise the role |
Once a business case has been approved, the role should be advertised. If it is a new role, there may not be suitable candidates therefore the role may need to be advertised as a ‘trainee’. This means that the employing organisation recognises the need to fund and provide the education and learning opportunities to develop the advanced level role. As per point 1, the role should be advertised for all registered practitioners who meet the essential criteria, not just dietitians. |
|
4. Recruit |
If the successful applicant has learning needs to meet the advanced level of practice, they will be recruited into a trainee role. The job description should reflect that they are in a trainee role working under supervision for the advanced level interventions they are learning. |
|
5. Training period |
The trainee should be supported by their employer to complete academic and workplace-based learning and assessment at Master's level. Depending on the role, this may be an advanced practice Master's. This training period is likely to be two to three years' duration. |
|
6. Transition |
On completion of the training period, the practitioner should be supported with a transition period (like foundation preceptorship) that allows them to transition from trainee to fully qualified practitioner. This could be from three to 12 months depending on the individual practitioner's situation. |
|
7. Deployment of advanced practice role |
Following the transition period, the job description should be changed to reflect the roles and responsibilities of the fully qualified advanced practice role. For indemnity insurance purposes, the job description should detail additional responsibilities being undertaken (such as endoscopy etc.) Governance of the roles must be provided through organisational structures that include a robust ongoing supervision structure. |